An Overview of Patient Transport Safety
During the COVID-19 pandemic, the role of EMS agencies in transporting patients expanded, allowing EMS services to take patients to alternative destinations.1 While it is too early to tell whether these adjustments might have a long-term impact, it’s important that all EMS personnel frequently refresh their knowledge on patient transport safety to help improve outcomes. Developing safe transport skills and knowledge is crucial for workplace safety for EMTs, EMRs, paramedics, and other EMS professionals as well as the safety of our patients.
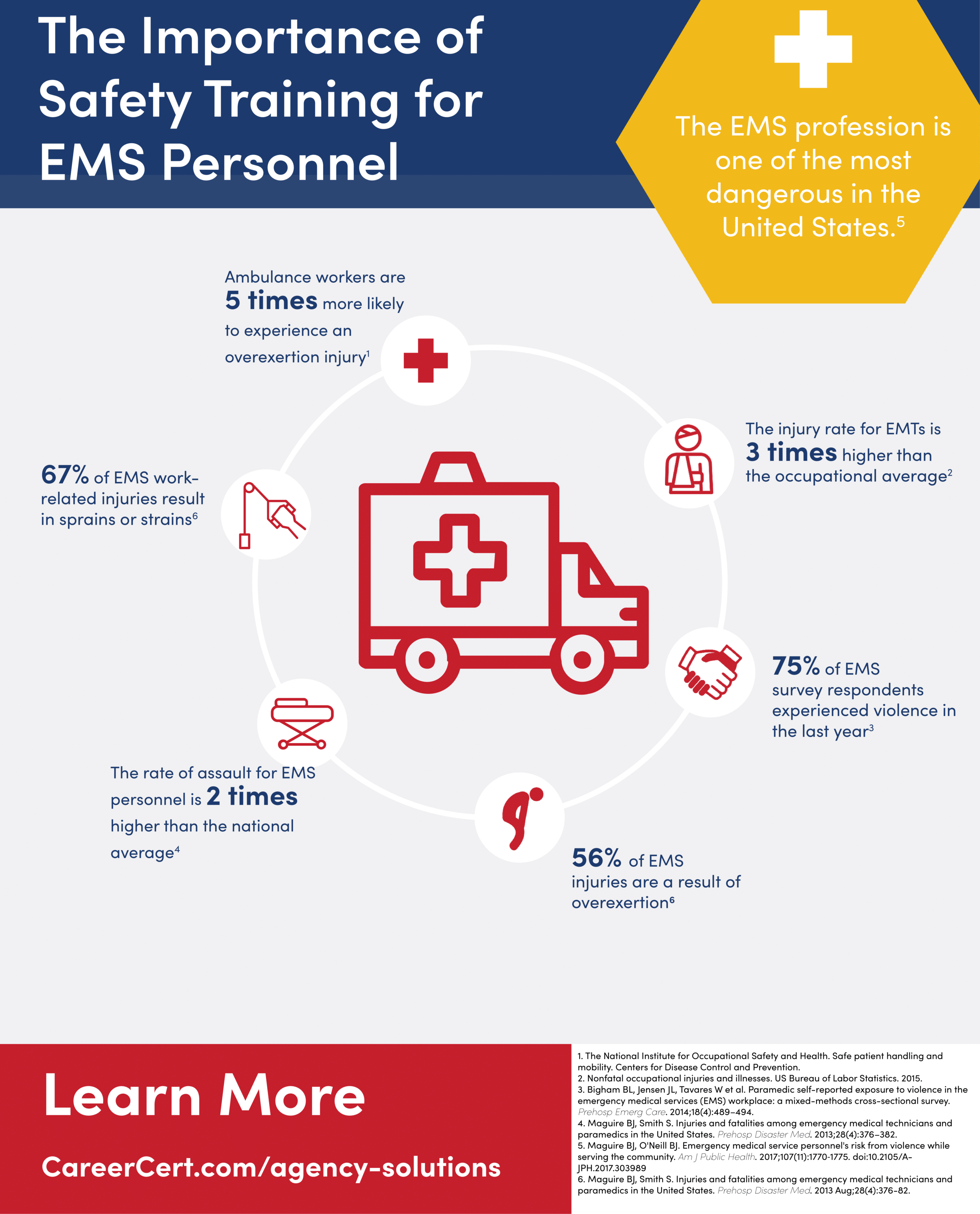
In addition to preparing for potential disasters, EMS personnel must also be prepared to face daily hazards. For example, incidents of paramedic assault in the United States are rising. According to the Occupational Health and Safety Administration (OSHA), approximately 75% of workplace assaults reported annually occurred in healthcare and social service settings.2
Other hazards include increased risk of exposure, heat, potential for physical injury, environmental and occupational stressors, and more.
Best Practices for Vehicle Operators
 A 2011 study in Prehospital Emergency Care found that 45% of fatal injuries for EMS professionals were due to motor vehicle collisions, with an additional 12% of fatalities involving personnel being struck by moving vehicles.3
A 2011 study in Prehospital Emergency Care found that 45% of fatal injuries for EMS professionals were due to motor vehicle collisions, with an additional 12% of fatalities involving personnel being struck by moving vehicles.3
Additionally, a recent analysis of two decades of data by the National Highway Traffic Safety Administration (NHTSA) showed that ambulances are involved in 10,000 crashes each year.4
Improving patient transport safety and the safety of our brothers and sisters in the service starts with the vehicle operator. There are many things agencies can do to help vehicle operators understand their responsibilities and carry them out effectively, including:4
- Study and comply with federal, state, and local vehicle safety regulations
- As an agency, determine and share clear performance expectations for vehicle operators
- Provide access to EMS driving courses and training
- Have vehicle operators contribute and participate in vehicle maintenance
- Set a standard where both the vehicle operator and their partner share responsibility for the safety of the team, patients, and the vehicle
- In case of a vehicle incident, carry out a full investigation to determine causes and contributing factors and fully document actions to prevent the incident from repeating
One seemingly obvious and yet often overlooked best practice in patient transport safety is the use of seatbelts. A study by the NHTSA found that “only 16% of EMS practitioners in the patient compartment at the time of a serious collision were wearing seatbelts. The rest (84%) were unrestrained, while 22% of the drivers were not wearing seatbelts.”5
Safe driving to and from emergency incidents can also be improved by increasing the vehicle operator’s situational awareness. Some suggestions include:4
- Predicting and understanding the effects of weather on the road, including rain, snow, and fog
- Both the driver and his or her partner should continuously scan the road for potential hazards
- Driver distractions like eating, drinking, grooming, using the phone, using the radio, or using a GPS should be prohibited. Navigation and communication should be handled by the partner who is not operating the vehicle.
- The vehicle operator’s partner can check the right-side blind spots of the vehicle for the driver.
- Unless the vehicle operator’s partner is caring for a patient, they should exit the vehicle and check the entire surrounding area for hazards before backing up. After determining the area is clear of hazards, they should direct the driver from the rear.
Best Practices for Transporting Patients
The following are best practices that can be put into effect immediately to ensure that patients are safe and secure during transport:
- EMS professionals in the patient compartment should wear seatbelts at all times, except when they are momentarily performing specific treatment on a patient. This prevents falling on or otherwise injuring a patient while the vehicle is in motion.
- Mothers should not hold children in the back of the vehicle. Children should be properly restrained based on their age and medical needs.
- Patients should be secured on a gurney with the restraint system and safety straps in place in line with the manufacturer’s recommendations.
- Patients in a wheelchair should be belted into their wheelchair with the wheelchair secured to the vehicle. A supplemental restraint device like a shoulder strap should also be engaged.
- EMS personnel should be well-trained and continuously review essential medical skills. In addition, they should receive training on situational awareness, how to recognize and mitigate dangerous situations, how to de-escalate stressful situations, how to treat violent or belligerent patients or bystanders, how to manage mental health changes and mood swings, etc.
Transporting Violent Patients
Research into how to best work with, prevent harm by, and transport violent patients is still evolving. For too long, violence from patients was an accepted hazard of the job for EMS professionals, but it does not have to be.
Patients can react violently for a number of reasons, including an uncontrolled psychological response to trauma. To help you handle such situations, here are a few practices that can be applied to discourage or mitigate violent behavior from patients:6
- Take advantage of free online training and self-defense courses like those offered by the National Institute for Occupational Safety and Health.
- Place signage in the back of each emergency vehicle that reminds patients that it is a felony to assault a first responder.
- Improve communication between departments that can prepare first responders for a possible violent situation. Some dispatch systems use a flag to alert EMS workers if their destination is the site of a patient-initiated violent injury. Using codes can also be an effective way to communicate worries or concerns without alerting patients.
- Create a safe environment for EMS professionals to report incidents and provide them with support during legal proceedings if an assault does occur.
Sources
- Wirth S, Stark R. Temporary CMS changes provide needed flexibility. EMS1. Apr 1, 2020. https://www.ems1.com/transport/articles/temporary-cms-changes-provide-needed-flexibility-GaDG26aWKluQFPOq/.
- Occupational Safety and Health Administration. Guidelines for preventing workplace violence for healthcare and social service workers (OSHA, 3148-04R). Washington, DC: OSHA, 2015.
- Reichard AA. Fatal and nonfatal injuries among emergency medical technicians and paramedics. Prehospital Emergency Care. Aug 11, 2011. https://www.ncbi.nlm.nih.gov/pubmed/21834620.
- Guide for developing an EMS agency safety program. National EMS Safety Council. Oct 11, 2017. http://www.naemt.org/docs/default-source/ems-health-and-safety-documents/nemssc/ems-safety-program-guide-10-11-17.p.
- Smith N. A national perspective on ambulance crashes and safety. EMSWorld.com. Sept 2015. https://www.ems.gov/pdf/EMSWorldAmbulanceCrashArticlesSept2015.pdf.
- Violence against EMS responders. U.S. Fire Administration. Aug 31, 2017. https://www.usfa.fema.gov/current_events/083117.html.


