Handling Field Opioid Incidents in Fire
 The opioid crisis is quickly touching every aspect of American life. As first responders, we know this better than anyone. We are on the frontlines witnessing and responding to calls related to opioid incidents.
The opioid crisis is quickly touching every aspect of American life. As first responders, we know this better than anyone. We are on the frontlines witnessing and responding to calls related to opioid incidents.
As the epidemic grows and communities work together to find solutions, fire professionals are an essential part of the opioid crisis response.
Progression of the Opioid Crisis
Opioids include prescription pain medications, heroin, and synthetic drugs like fentanyl.
From 1999 to 2017, almost 400,000 people died from an overdose involving opioids, including prescription and illicit opioids. This rise in opioid overdose deaths and this crisis can be outlined in 3 distinct waves:
- The first wave began with increased prescribing of opioids in the 1990s, with overdose deaths involving prescription opioids (natural and semi-synthetic opioids and methadone) increasing since at least 1999.
- The second wave began in 2010, with rapid increases in overdose deaths involving heroin.
- The third wave began in 2013, with significant increases in overdose deaths involving synthetic opioids—particularly those involving illicitly manufactured fentanyl (IMF). The IMF market continues to change, and IMF can be found in combination with heroin, counterfeit pills, and cocaine.
The Current Opioid Crisis
The newest wave involves an uptick in unregulated synthetic drugs readily sold over the internet, compounding the crisis on a number of levels. Much stronger strains of fentanyl and unidentified new chemical compounds are manufactured and shipped to the US and other countries.
The latest data from the National Institute on Drug Abuse shows that 128 people in the United States die each day after overdosing on opioids.
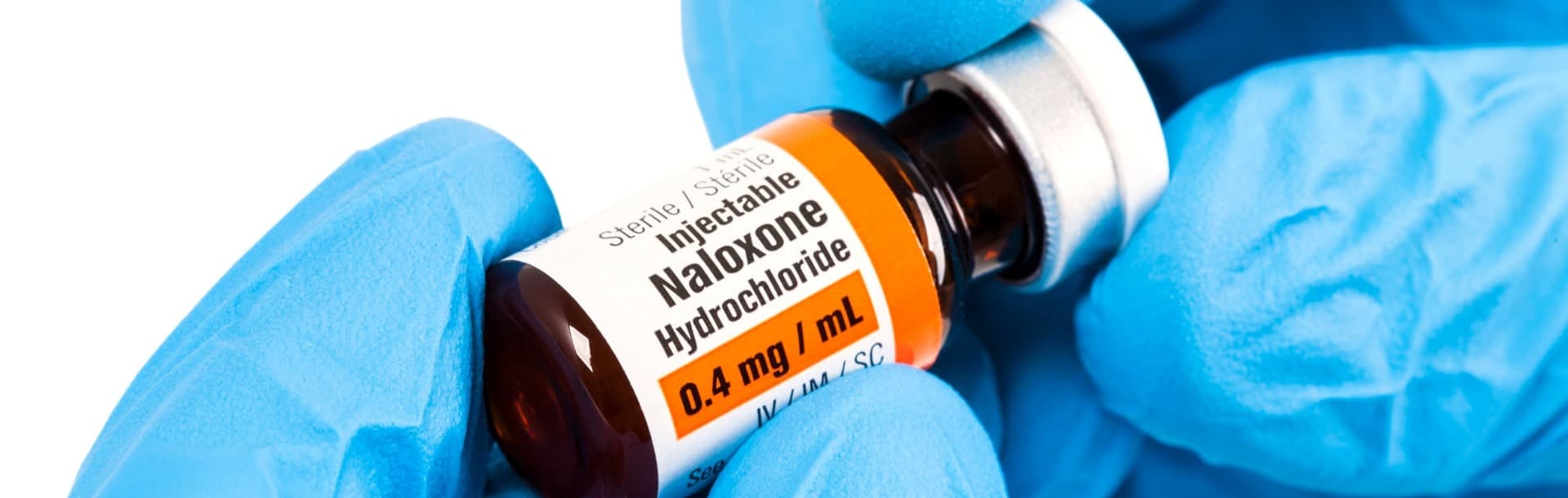
Government leaders, emergency responders, and healthcare providers have taken steps to try to prevent opioid abuse and addiction. Protocols like patient-controlled analgesia aim to prevent overdoses and help patients self-administer within safe limits. First responders have more easy access to and training in administering Naloxone, which can rapidly reverse opioid overdoses and save lives.
The most common drugs involved in prescription opioid overdose deaths include methadone, oxycodone, and hydrocodone
Prescription opioid overdose deaths also often involve benzodiazepines, which are central nervous system depressants used to promote sleep, prevent seizures, relieve anxiety, and sedate (such as Xanax and Valium).
Firefighters’ Role in Opioid Incidents
Mark Lockhart, fire and EMS chief for Stafford County, Virginia, says, “The fire service is an all-hazard service—if there is a threat to life or property, we are duty-bound to handle it when we are called. We’re on the frontline of [the opioid crisis].”
As the opioid epidemic has evolved, the role we play as firefighters has evolved as well. Many departments are having to adjust how they allocate resources.
Learning about the signs and symptoms of an overdose is essential to connecting patients with the appropriate care. The signs and symptoms of opioid overdose include:
- Face extremely pale and/or clammy to the touch
- Body goes limp
- Fingernails or lips have a purple or blue color
- Vomiting or making gurgling noises
- Cannot be awakened or unable to speak
- Breathing or heartbeat slows or stops
It’s also important for us as firefighters to understand potential hazards that might arise when called to the scene of an opioid overdose. As Critical Care Paramedic and instructor Kuo Downing-Reese notes, carfentanil is often mixed with other drugs to produce a deeper feeling of analgesia or “high.” She says:
“Carfentanil was originally designed for analgesia of large mammals, such as elephants, but in recent years has found its way into the illegal drug world. This new adoption of carfentanil exposes first responders to the very serious risk of overdose themselves. The smallest amount, less than the size of a penny, in contact with the skin can cause overdose. First responders should remain vigilant whenever a white powder is present on scene.”
In addition, patients who have experienced an opioid overdose are more likely to become violent or combative, which is why maintaining situational awareness is key to safety for all on scene.
The increase in opioid-related calls makes it crucial for emergency teams to have access to in-depth fire continuing education (fire CE) that tackles this issue. In searching for training for your team or for yourself, be sure to invest in training from industry experts that is up-to-date and as current as possible. Especially for emerging industry topics, it’s crucial to have access to the latest research and best practices.
Providing Better Care and Response
What can fire professionals do to provide better care and smooth handling of opioid incidents in the field? Lockhart says, “Training, training, training.” In your own stations and as part of fire CE, educate your team on the global opioid crisis. Assess threats to your current mode of operation, like increased call volume and health and safety concerns for firefighters responding to opioid incidents.
Fire leaders should also recognize that no one is safe from this crisis. Even firefighters can fall victim to opioid addictions, especially because the physical nature of our job makes us more prone to injury. Know the signs of those struggling with addiction and appropriate ways to reach out and help. According to Johns Hopkins Medicine, these include:
- The inability to control opioid use
- Uncontrollable cravings
- Drowsiness
- Changes in sleep habits
- Weight loss
- Frequent flu-like symptoms
- Decreased libido
- Lack of hygiene
- Changes in exercise habits
- Isolation from family or friends
- Stealing from family, friends or businesses
- New financial difficulties
Get involved with local community leaders and task forces to coordinate prevention and treatment efforts.
The opioid crisis has also created an opportunity for firefighters to step into their role as community educators and as a support for those who are struggling. For example, Anne Arundel County in Maryland has designated all of its fire stations as safe stations for those looking for help with managing and overcoming opioid addiction. Staff are trained in assessment, treatment, and how to activate a system of community resources to quickly get those who come into the station into drug treatment.
As law enforcement, first responders, mental health services, and social services work together, response and prevention can improve and together we can fight to overcome opioid addiction in our communities.
For effective online training to help you or your team prepare for opioid-related incidents and prevent drug abuse, check out CareerCert’s courses that allow you to earn CEs and refresh your skills anytime, anywhere, and on any device. To access CareerCert’s industry-leading opioid training online, log into your account or check out our pricing options.
Sources
- Bunker D. U.S. opioid epidemic: Misconceptions and prevention. April 2020. https://careercert.com/articles/other-medical-concerns/u-s-opioid-epidemic-misconceptions-and-prevention/.
- Downing-Reese K. Naloxone in EMS: Narcan administration for opioid overdose. May 2020. https://careercert.com/articles/other-medical-concerns/naloxone-in-ems-narcan-administration-and-side-effects/.
- Hatt K. Q&A: Why the opioid epidemic is a fire service issue. FireRescue1. Apr. 4, 2018. https://www.firerescue1.com/combating-the-opioid-crisis/articles/qa-why-the-opioid-epidemic-is-a-fire-service-issue-4QnEWTcBJ1lQtv17/.
- Johns Hopkins Medicine. Signs of opioid abuse. https://www.hopkinsmedicine.org/opioids/signs-of-opioid-abuse.html.
- National Institute on Drug Abuse. Opioid overdose crisis. NIH. February 2020. https://www.drugabuse.gov/drugs-abuse/opioids/opioid-overdose-crisis
- Opioid overdose. Centers for Disease Control and Prevention. March 19, 2020. https://www.cdc.gov/drugoverdose/epidemic/index.html.