Integrating Technology into Quality Pre-Hospital and Hospital Improvement Training
Synopsis
“Quality improvement is not a static concept, but rather a continually emerging, dynamic system property.”—World Health Organization
Due to the dynamic nature of healthcare, solutions to improve patient outcomes must be similarly dynamic. Instead of meeting baseline requirements, effective training that can improve community outcomes should focus on evidence-based education geared at quality improvement. Emerging online technologies provide new avenues to make this level of training more accessible and adaptable than ever before.
Introduction
Healthcare is a dynamic, evolving industry. In “Challenges and opportunities facing medical education,” Peter Densen estimates that the world’s medical knowledge doubled every 73 days in 2020.1 Keeping pace with the rapid growth of knowledge is compounded by the challenge of keeping pace with emerging healthcare technologies. “Emerging medical devices and technologies, especially the mobile phones and tiny Nano-sized sensors embedded in several electronic devices that enable sending and receiving information wirelessly, are changing the face of 21st Century medical practice,” Mohammad Bajwa notes in “Emerging 21st Century Medical Technologies.”2
The gaps between emerging medical knowledge and technologies and current provider understanding directly impact patient outcomes and medical costs. Medical error is the third leading cause of death in the United States,3 and approximately 400,0000 hospitalized patients every year experience preventable harm.4 In 2018, the World Health Organization (WHO) revealed that 15% of hospital expenditure in high-income countries is due to mistakes (which equated to $178.8 billion in the U.S. in 2018) and that 20% of health resources are used in ways that don’t make improvements.5 Some estimates of medical error rise to as high as $1 trillion annually when quality-adjusted life years are taken into account.6
Due to the dynamic nature of healthcare, solutions to improve patient outcomes and decrease medical costs must be similarly dynamic and multifaceted, not simplistic or static. Quality improvement measures need room to evolve to incorporate emerging training and technologies. As WHO notes, “Quality improvement is not a static concept, but rather a continually emerging, dynamic system property. Many different methods are used to continuously assure and improve the quality of healthcare, . . . A basic tenet underlying continuous quality improvement is activated learning mechanisms using iterative cycles of change.”5
Among the valuable learning mechanisms used to improve quality of care is training for medical providers.
Importance of Quality Training to Improve Outcomes
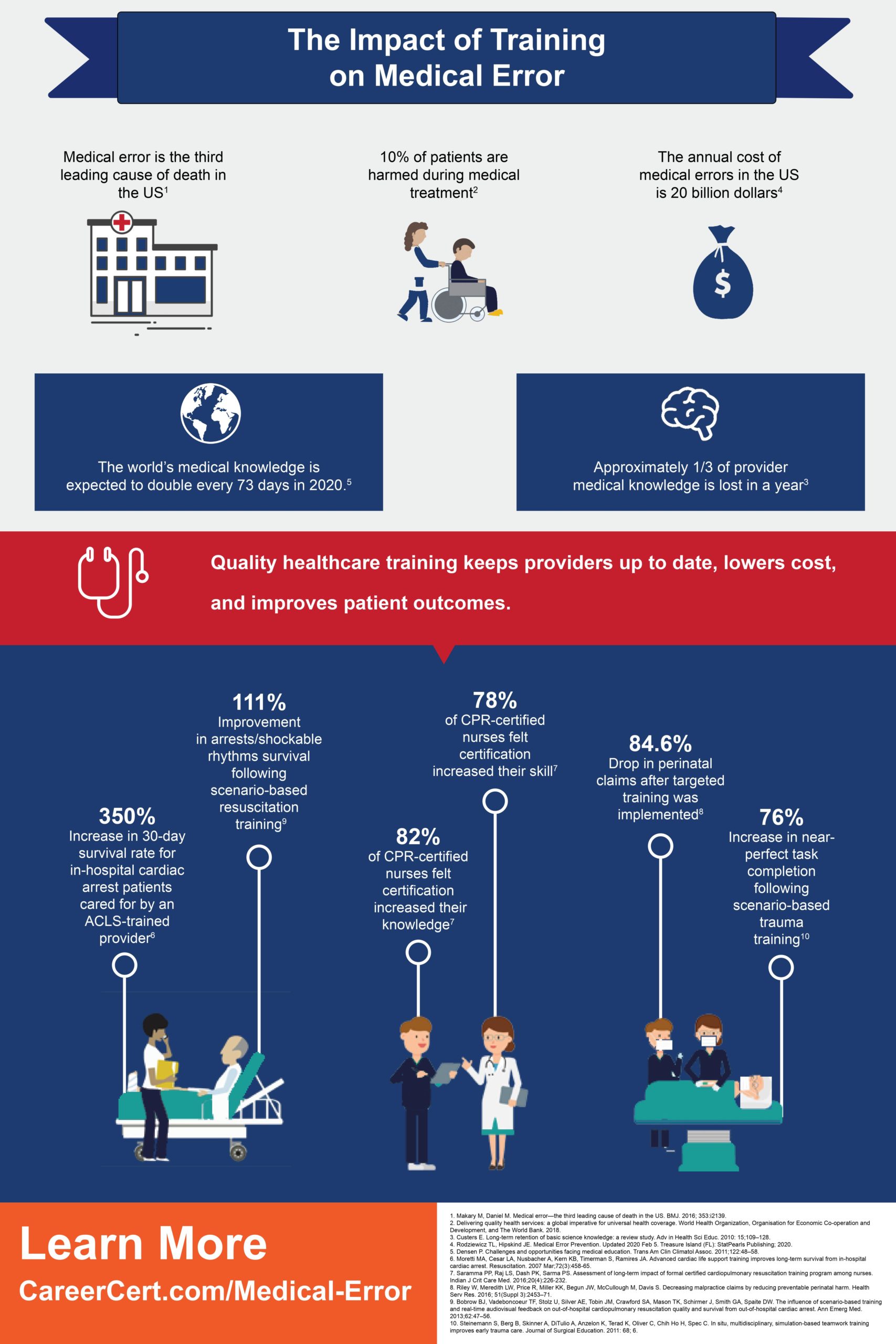 One of the root causes of medical error is “Deficiencies in education, training, orientation, and experience,”7 while quality healthcare education and training has been repeatedly demonstrated to improve patient outcomes.3
One of the root causes of medical error is “Deficiencies in education, training, orientation, and experience,”7 while quality healthcare education and training has been repeatedly demonstrated to improve patient outcomes.3
Within healthcare, continual, consistent training is needed not only to introduce new medical best practices but also to combat the loss of provider knowledge over time. “The estimated percentages of how much information learners forget after the initial learning period varies, with most estimates falling between 75 and 98 percent,” M. Courtney Hughes writes in “The importance of training for memory retention.”8 However, Hughes also notes effective ways to improve retention and recall, including: 1) reintroducing materials, 2) activating information, and 3) spaced repetition.8
Training not only reinforces providers’ mental response in emergency situations, it also enhances psychological and physiological responses. In On Combat</em”>, Lt. Col. Dave Grossman discusses the body’s response in high-stress situations: heart rate increases, as does peripheral vasoconstriction, causing individuals to lose fine motor movement.9 In such situations, providers rely on muscle memory to perform critical tasks that could prove life-saving—muscle memory that can only be built through consistent practice and training.
To receive the necessary mental and physical benefits of training, active learning and quality improvement are essential ingredients in any effective program. In a study on quality improvement programs in the prehospital setting, Erin W. Lincoln et al. observe, “Compliance with system clinical guidelines and protocols . . . does not ensure continuous quality improvement. While compliance is critical to ensure baseline performance, these performance indicators will likely be indicative of any necessary changes to implement. Essentially, baseline protocol compliance and quality assurance can be paired with quality improvement projects and initiatives to improve clinical outcome.”10Improving patient outcomes incorporates more than meeting baseline protocols. It requires investing in innovative training that focuses on quality improvement.
As WHO notes, “Integrating the principles of quality and quality improvement into pre-service and in-service education and training curricula and programmes is vital in building a competent workforce that is capable of delivering high-quality health services.”5
In a previous article, I outlined specific examples of effective training programs that improved outcomes across multiple fields in a prehospital and hospital setting, including increasing near-perfect task completion rates in early trauma care by 76%,11 reducing neonatal hypoxic–ischaemic encephalopathy in infants by over 50%,12 improving CPR arrests/shockable rhythms survivals by 29.2%,13 and dropping the average amount of indemnity payments for perinatal claims by 84.6% per hospital.14 Common threads through each of these studies includes attention to:
- Quality, evidence-based education
- Scenario-based or simulation-based drills that physically and practically reinforce training concepts
- And feedback on provider performance
These components mirror Hughes’ formula for promoting provider retention and outline essential ingredients for training that have the leverage and potential to impact patient outcomes.
As Thomas L. Rodziewicz and John E. Hipskind succinctly summarize in Medical Error Prevention, “Teamwork, education, and training through structured initiatives are the most effective mechanism to improve patient safety.”7
Sources
- Densen P. Challenges and opportunities facing medical education. Trans Am Clin Climatol Assoc. 2011;122:48–58.
- Bajwa M. Emerging 21(st) Century Medical Technologies. Pak J Med Sci. 2014;30(3):649–655. doi:10.12669/pjms.303.5211
- Makary M, Daniel M. Medical error—the third leading cause of death in the US. BMJ. 2016; 353:i2139. https://doi.org/10.1136/bmj.i2139.
- Rodziewicz TL, Hipskind JE. Medical Error Prevention. Updated 2020 Feb 5. Treasure Island (FL): StatPearls Publishing; 2020. https://www.ncbi.nlm.nih.gov/books/NBK499956/.
- Delivering quality health services: a global imperative for universal health coverage. Geneva: World Health Organization, Organisation for Economic Co-operation and Development, and The World Bank; 2018.
- Andel C, Davidow SL, Hollander M, Moreno DA. The economics of health care quality and medical errors. J Health Care Finance. 2012;39(1):39–50.
- Rodziewicz TL, Hipskind JE. Medical Error Prevention. Updated 2020 Feb 5. Treasure Island (FL): StatPearls Publishing; 2020.
- Hughes MC. The importance of training for memory retention. Training Magazine. 2018 Jun 18. https://trainingmag.com/importance-training-memory-retention/.
- Grossman D., Christensen LW. On combat: the psychology and physiology of deadly conflict in war and in peace. Illinois: Warrior science publ. 2008
- Lincoln EW, Reed-Schrader E, Jarvis JL. EMS, quality improvement programs. Updated 2019 Jul 28. Treasure Island (FL): StatPearls Publishing; 2020.
- Steinemann S, Berg B, Skinner A, DiTulio A, Anzelon K, Terad K, Oliver C, Chih Ho H, Spec C. In situ, multidisciplinary, simulation-based teamwork training improves early trauma care. Journal of Surgical Education. 2011: 68; 6.
- Draycott T, Sibanda T, Owen L, Akande V, Winter C, Reading S, Whitelaw A. Does training in obstetric emergencies improve neonatal outcome? BJOG: An International Journal of Obstetrics & Gynaecology. 2006. 113: 177-182. doi:10.1111/j.1471-0528.2006.00800.x.
- Bobrow BJ, Vadeboncoeur TF, Stolz U, Silver AE, Tobin JM, Crawford SA, Mason TK, Schirmer J, Smith GA, Spaite DW. The influence of scenario-based training and real-time audiovisual feedback on out-of-hospital cardiopulmonary resuscitation quality and survival from out-of-hospital cardiac arrest. Ann Emerg Med. 2013;62:47–56. doi: 10.1016/j.annemergmed.2012.12.020.
- Riley W, Meredith LW, Price R, Miller KK, Begun JW, McCullough M, Davis S. Decreasing malpractice claims by reducing preventable perinatal harm. Health Serv Res. 2016; 51(Suppl 3):2453–71.