An Overview of Hepatitis A, B, C, D & E for Medical Providers
 Hepatitis defined in its most simple form is inflammation of the liver. This inflammation is often caused by one of several viruses—hepatitis A virus (HAV), hepatitis B virus (HBV), hepatitis C virus (HCV), hepatitis D virus (HDV), and hepatitis E virus (HEV). Other causes of hepatitis are heavy alcohol use, toxins, some medications, and certain medical conditions. The most common types of hepatitis are A, B, and C.
Hepatitis defined in its most simple form is inflammation of the liver. This inflammation is often caused by one of several viruses—hepatitis A virus (HAV), hepatitis B virus (HBV), hepatitis C virus (HCV), hepatitis D virus (HDV), and hepatitis E virus (HEV). Other causes of hepatitis are heavy alcohol use, toxins, some medications, and certain medical conditions. The most common types of hepatitis are A, B, and C.
The following information was obtained from the Center for Disease Control and Prevention’s website dedicated to viral hepatitis. The information has been consolidated for this article primarily for the use of healthcare providers who have some base knowledge of viral hepatitis.
Hepatitis A
Clinical Criteria
An acute illness with a discrete onset of any sign or symptom consistent with acute viral hepatitis (e.g. fever, headache, malaise, anorexia, nausea, vomiting, diarrhea, abdominal pain, or dark urine) AND a) jaundice or elevated total bilirubin levels ≥ 3.0 mg/dL, OR b) elevated serum alanine aminotransferase (ALT) levels >200 IU/L AND c) the absence of a more likely diagnosis.
Laboratory Criteria for Diagnosis
Confirmatory laboratory evidence: Immunoglobulin M (IgM) antibody to hepatitis A virus (anti-HAV) positive, OR nucleic acid amplification test (NAAT; such as polymerase chain reaction [PCR] or genotyping) for hepatitis A virus RNA positive.
Transmission
Hepatitis A is transmitted through the fecal-oral route:
- Close person-to-person contact with an infected person
- Sexual contact with an infected person
- Ingestion of contaminated food or water
Signs and Symptoms
- Fever
- Fatigue
- Nausea
- Vomiting
- Abdominal pain
- Dark urine
- Diarrhea
- Clay-colored stool
- Joint pain
- Jaundice
Risk of Becoming Chronic Disease
Hepatitis A does not become a chronic, long-term infection.
Prevention
Vaccination with the full, 2-dose series of hepatitis A vaccine is the best way to prevent infection.
Healthcare Providers
Hepatitis A vaccine is not routinely recommended for healthcare personnel, because healthcare-associated transmission of hepatitis A virus is rare in the United States.
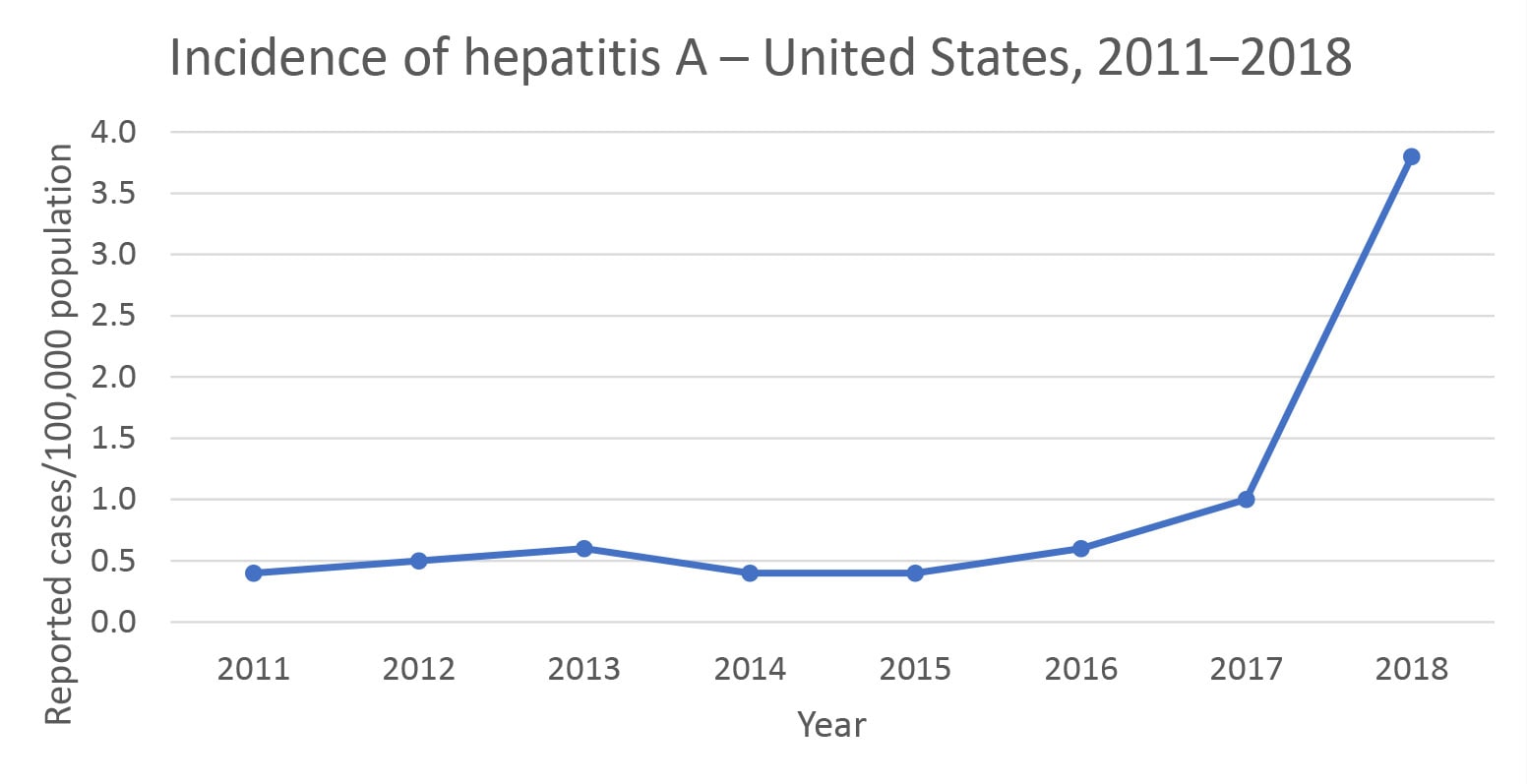
Incidence of Hepatitis A in the United States
Post-Exposure/Treatment
Hepatitis A vaccine should be administered as soon as possible, within 2 weeks of exposure, to all unvaccinated people aged ≥12 months who have recently been exposed to hepatitis A virus (HAV). In addition to hepatitis A vaccine, co-administration of GamaSTAN S/D immune globulin (0.1 mL/kg) is recommended under certain circumstances, according to the age and health status of the exposed person.
Hepatitis B
Clinical Criteria
Acute Hepatitis B
An acute illness with a discrete onset of any sign or symptom consistent with acute viral hepatitis (e.g. fever, headache, malaise, anorexia, nausea, vomiting, diarrhea, and abdominal pain), AND either a) jaundice, OR b) elevated serum alanine aminotransferase (ALT) levels >100 IU/L.
Chronic Hepatitis B
No symptoms are required. Persons with chronic hepatitis B virus (HBV) infection may have no evidence of liver disease or may have a spectrum of disease ranging from chronic hepatitis to cirrhosis or liver cancer.
Laboratory Criteria for Diagnosis
Acute Hepatitis B
HBsAg positive, AND Immunoglobulin M (IgM) antibody to hepatitis B core antigen (IgM anti-HBc) positive (if done).
Chronic Hepatitis B
Immunoglobulin M (IgM) antibodies to hepatitis B core antigen (IgM anti-HBc) negative AND a positive result on one of the following tests: hepatitis B surface antigen (HBsAg), hepatitis B e antigen (HBeAg), or nucleic acid test for hepatitis B virus DNA (including qualitative, quantitative, and genotype testing), OR HBsAg positive or nucleic acid test for HBV DNA positive (including qualitative, quantitative, and genotype testing), OR HBeAg positive 2 times at least 6 months apart. (Any combination of these tests performed 6 months apart is acceptable.)
Transmission
HBV is transmitted through activities that involve percutaneous (i.e. puncture through the skin) or mucosal contact with infectious blood or body fluids (e.g. semen and saliva), including:
- Sex with an infected partner;
- Injection-drug use that involves sharing needles, syringes, or drug-preparation equipment;
- Birth to an infected mother;
- Contact with blood from or open sores on an infected person;
- Exposures to needle sticks or sharp instruments; and
- Sharing certain items with an infected person that can break the skin or mucous membranes (e.g. razors, toothbrushes, and glucose monitoring equipment), potentially resulting in exposure to blood.
Signs and Symptoms
Acute Hepatitis B
Not all people with acute HBV infection have symptoms. Those that do include:
- Fever
- Fatigue
- Loss of appetite
- Nausea
- Vomiting
- Abdominal pain
- Dark urine
- Clay-colored stool
- Joint pain
- Jaundice
Chronic Hepatitis B
Most people with chronic HBV infection are asymptomatic and have no evidence of liver disease or injury. However, some people develop chronic hepatitis (elevation of AST/ALT), cirrhosis, or hepatocellular carcinoma (i.e. primary liver cancer).
Risk of Becoming Chronic
The risk for chronic infection varies according to the age at infection and is greatest among young children. Approximately 90% of infants and 25%–50% of children aged 1–5 years will remain chronically infected with HBV. By contrast, approximately 95% of adults recover completely from HBV infection and do not become chronically infected
Prevention
Vaccination is recommended to reduce the risk of HBV infection. The following groups should be vaccinated:
- All infants
- Unvaccinated children aged <19 years
- People at risk for infection by sexual exposure
- Sex partners of people testing positive for hepatitis B surface antigen (HBsAg)
- Sexually active people who are not in a long-term, mutually monogamous relationship (e.g. people with more than one sex partner during the previous 6 months)
- People seeking evaluation or treatment for a sexually transmitted infection
- Men who have sex with men
- People at risk for infection by percutaneous or mucosal exposure to blood
- People who currently inject or have recently injected drugs
- Household contacts of people who are HBsAg-positive
- Residents and staff of facilities for developmentally disabled people
- Healthcare and public safety personnel with reasonably anticipated risk for exposure to blood or blood-contaminated body fluids
- Hemodialysis patients and predialysis, peritoneal dialysis, and home dialysis patients
- People with diabetes aged 19–59 years; people with diabetes aged ≥60 years at the discretion of the treating clinician
- International travelers to countries with high or intermediate levels of endemic hepatitis B virus (HBV) infection (HBsAg prevalence of ≥2%)
- People with hepatitis C virus infection
- People with chronic liver disease (including, but not limited to, people with cirrhosis, fatty liver disease, alcoholic liver disease, autoimmune hepatitis, and an alanine aminotransferase [ALT] or aspartate aminotransferase [AST] level greater than twice the upper limit of normal)
- People with HIV infection
- People who are incarcerated
- All other people seeking protection from HBV infection
Healthcare Providers
In certain healthcare, evaluation, or treatment settings, a high proportion of clients have known risk factors for HBV infection:
- Sexually transmitted disease treatment facilities
- HIV testing and treatment facilities
- Facilities providing drug-abuse treatment and prevention services
- Healthcare settings targeting services to people who inject drugs
- Correctional facilities
- Healthcare settings targeting services to men who have sex with men
- Chronic hemodialysis facilities and end-stage renal disease programs
- Institutions and nonresidential day-care facilities for people with developmental disabilities
Incidence of Hepatitis B in the United States
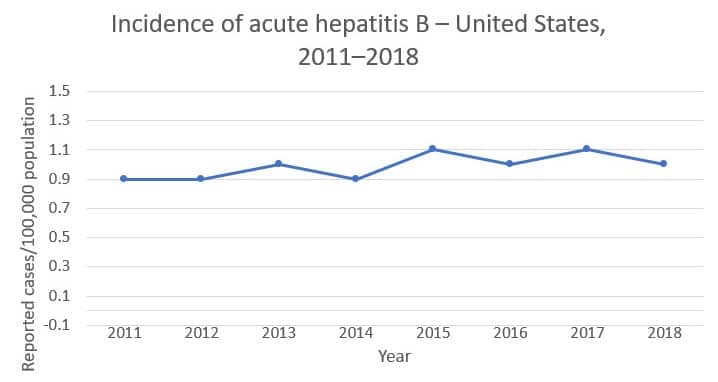
In 2016, an estimated 862,000 people were living with HBV infection.
Post-Exposure/Treatment
People with acute infection are provided supportive treatment depending on their symptoms. For people with chronic infection, several antiviral medications are available; these patients require linkage to care with regular monitoring to prevent liver damage and/or hepatocellular carcinoma.
Hepatitis C
Clinical Criteria
Acute and Chronic Hepatitis C
All hepatitis C virus cases in each classification category should be > 36 months of age, unless known to have been exposed non-perinatally.
One or more of the following is used for diagnosis: jaundice, OR peak elevated total bilirubin levels ≥ 3.0 mg/dL, OR peak elevated serum alanine aminotransferase (ALT) levels >200 IU/L AND the absence of a more likely diagnosis (which may include evidence of acute liver disease due to other causes or advanced liver disease due to pre-existing chronic hepatitis C virus (HCV) infection or other causes, such as alcohol exposure, other viral hepatitis, hemochromatosis, etc.)
Laboratory Criteria for Diagnosis
Acute and Chronic Hepatitis C
Confirmatory laboratory evidence:
- Positive hepatitis C virus detection test: Nucleic acid test (NAT) for HCV RNA positive (including qualitative, quantitative, or genotype testing), OR
- A positive test indicating presence of hepatitis C viral antigen(s) (HCV antigen)
Presumptive laboratory evidence:
- A positive test for antibodies to hepatitis C virus (anti-HCV)
Transmission
HCV is transmitted primarily through parenteral exposures to infectious blood or body fluids that contain blood. Possible exposures include:
- Injection-drug use (currently the most common mode of HCV transmission in the United States)
- Birth to an HCV-infected mother
Although less frequent, HCV can also be spread through:
- Sex with an HCV-infected person (an inefficient means of transmission, although HIV-infected men who have sex with men have increased risk of sexual transmission)
- Sharing personal items contaminated with infectious blood, such as razors or toothbrushes
- Other healthcare procedures that involve invasive procedures, such as injections (usually recognized in the context of outbreaks)
- Unregulated tattooing
- Receipt of donated blood, blood products, and organs (rare in the United States since blood screening became available in 1992)
- Needlestick injuries in healthcare settings
Signs and Symptoms
Acute Hepatitis C
People with newly acquired HCV infection usually are asymptomatic or have mild symptoms that are unlikely to prompt a visit to a healthcare professional. When symptoms do occur, they can include:
- Fever
- Fatigue
- Dark urine
- Clay-colored stool
- Abdominal pain
- Loss of appetite
- Nausea
- Vomiting
- Joint pain
- Jaundice
Chronic Hepatitis C
Most people with chronic HCV infection are asymptomatic or have non-specific symptoms such as chronic fatigue and depression. Many eventually develop chronic liver disease, which can range from mild to severe, including cirrhosis and liver cancer. Chronic liver disease in HCV-infected people is usually insidious, progressing slowly without any signs or symptoms for several decades.
Some people with chronic HCV infection develop medical conditions due to hepatitis C that are not limited to the liver. Such conditions can include:
- Diabetes mellitus
- Glomerulonephritis
- Essential mixed cryoglobulinemia
- Porphyria cutanea tarda
- Non-Hodgkin’s lymphoma
Risk of Becoming Chronic
More than half of people who become infected with HCV will develop chronic infection. A person infected with HCV mounts an immune response to the virus, but replication of the virus during infection can result in changes that evade the immune response. This may explain how the virus establishes and maintains chronicity.
Prevention
There is no vaccine for hepatitis C. The best way to prevent hepatitis C is by avoiding behaviors that can spread the disease, especially injecting drugs. Getting tested for hepatitis C is important because treatments can cure most people with hepatitis C in 8 to 12 weeks.
Healthcare Providers
Avoiding occupational exposure to blood is the primary way to prevent transmission of bloodborne illnesses among healthcare personnel. To promote blood safety in the workplace, healthcare personnel should consult infectious-disease control guidance from the National Institute for Occupational Safety and Health and from the CDC. Depending on the medical procedure involved, standard precautions may include the appropriate use of personal protective equipment (e.g. gloves, masks, and protective eyewear).
Incidence of Hepatitis C in the United States
Incidence rates of reported acute hepatitis C cases ── United States, 2000–2017
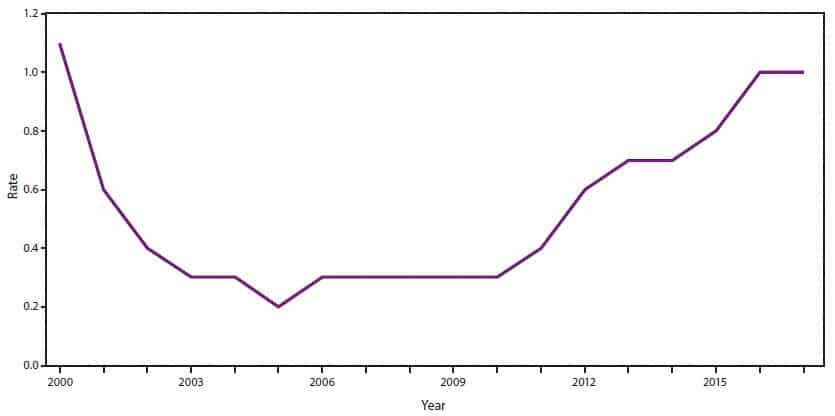
CDC, National Notifiable Diseases Surveillance System. Per 100,000 population.
Post-Exposure
The CDC does not recommend postexposure prophylaxis (PEP) for healthcare personnel exposed to hepatitis C virus (HCV)-contaminated blood. Instead, the source patient in question should be tested for HCV RNA or hepatitis C antibodies. For healthcare workers exposed to a patient testing positive for hepatitis C infection, or whose status remains unknown, management should be guided by the CDC’s testing algorithm. Healthcare workers who become infected with HCV should be managed and provided treatment according to AASLD/IDSA guidelines.
Hepatitis D
Hepatitis D is a liver disease caused by the hepatitis D virus (HDV). HDV is known as a satellite virus because it can only infect people who are also infected by the hepatitis B virus (HBV). HDV infection can be acute or lead to chronic, long-term illness. The infection can be acquired either simultaneously with HBV as a coinfection or as a superinfection in people who are already chronically infected with HBV.
Clinical and Laboratory Criteria for Diagnosis
Because cases of hepatitis D are not clinically distinguishable from other types of acute viral hepatitis, diagnosis can be confirmed only by testing for the presence of antibodies against HDV and/or HDV RNA. HDV infection should be considered in any person with a positive hepatitis B surface antigen (HBsAg) who has severe symptoms of hepatitis or acute exacerbations.
Transmission
HDV is mainly transmitted through activities that involve percutaneous (i.e. puncture through the skin) and to a lesser extent through mucosal contact with infectious blood or body fluids (e.g. semen and saliva), including:
- Sex with an infected partner
- Injection-drug use that involves sharing needles, syringes, or drug-preparation equipment
- Birth to an infected mother (rare)
- Contact with blood from or the open sores of an infected person
- Needle sticks or exposures to sharp instruments
- Sharing items (e.g. razors and toothbrushes) with an infected person
Signs and Symptoms
HDV causes infection and clinical illness only in HBV-infected people. The signs and symptoms of acute HDV infection are indistinguishable from those of other types of acute viral hepatitis infections. These include:
- Fever
- Fatigue
- Loss of appetite
- Nausea
- Vomiting
- Abdominal pain
- Dark urine
- Clay-colored bowel movements
- Joint pain
- Jaundice
These signs and symptoms typically appear 3–7 weeks after initial infection.
Acute hepatitis occurs in HBV/HDV coinfected people, and their symptoms may follow a biphasic course. Symptoms of HBV/HDV coinfection can range from mild to severe (fulminant hepatitis), but for most people, coinfection is self-limited: less than 5% of coinfected people go on to develop chronic infections. Regardless, acute liver failure is more common among people with HBV/HDV coinfection than among those infected with HBV alone.
HDV superinfection accelerates the progression of chronic HBV in 70%–90% of people, regardless of age. Although HDV suppresses the replication of HBV, cirrhosis occurs up to a decade earlier in HDV-superinfected persons compared with those infected with HBV alone. The mechanisms by which HDV accelerates progression and more severe disease are not clear.
Prevention
Although no vaccine is available for hepatitis D, vaccination with the hepatitis B vaccine can protect people from HDV infection.
Incidence of Hepatitis D in the United States
HDV infection is uncommon in the United States, where most cases occur among people who migrate or travel to the United States from countries with high HDV endemicity. Because hepatitis D is not a nationally notifiable condition, the actual number of hepatitis D cases in the United States is unknown
HBV/HDV coinfection occurs when a person simultaneously becomes infected with both HBV and HDV, whereas HDV superinfection occurs when a person who is already chronically infected with HBV acquires HDV. Although acute HBV/HDV coinfections can resolve, HDV superinfection can lead to rapid progression of the already present HBV infection, resulting in liver cirrhosis and liver failure. These outcomes occur within 5–10 years in 70%–80% and within 1–2 years in 15% of people with chronic HBV/HDV infection
Post-Exposure
No treatment is available for HDV infection specifically. Pegylated interferon alpha has shown some efficacy, but the sustained virologic response rate (a measure of viral clearance) is low (25%). New therapies are being evaluated. In cases of fulminant hepatitis and end-stage liver disease, liver transplantation may be considered.
Hepatitis E
Hepatitis E is a liver disease caused by the hepatitis E virus (HEV). Although rare in developed countries, hepatitis E is widespread in the developing world. In the vast majority of people, HEV infection results in a self-limited, acute illness. However, acute infection can become chronic in rare cases, primarily in people who have received solid-organ transplants.
Clinical Criteria
HEV is unique, in that it has a different clinical and epidemiologic profile depending on where the infection is acquired. This can be attributed largely to the viral genotypes circulating in different parts of the world. Four genotypes of HEV cause illness in humans, each displaying different epidemiologic and clinical characteristics in developing and developed countries. Cases of hepatitis E typically present in one of two ways: either as large outbreaks and sporadic cases in areas where HEV is endemic (genotype 1 in Asia and Africa, genotype 2 in Mexico and West Africa, and genotype 4 in Taiwan and China) or as isolated cases in developed countries like the United States (genotype 3). Recently, a new genotype (genotype 7) was identified in a liver-transplant recipient from UAE with chronic hepatitis E virus infection who frequently consumed camel meat and milk.
Transmission
HEV is usually spread by the fecal-oral route. In developing countries, where HEV genotypes 1 and 2 predominate, the most common source of HEV infection is contaminated drinking water. In developed countries, sporadic cases of HEV genotype 3 have occurred following consumption of uncooked/undercooked pork or deer meat. Consumption of shellfish was a risk factor in a recently described outbreak that occurred among cruise ship passengers. HEV genotype 4, detected in China, Taiwan, and Japan, has also been associated with foodborne transmission.
Hepatitis E can infect certain mammals, and consumption of uncooked/undercooked meat or organs from infected animals can lead to foodborne transmission to humans. HEV RNA (genotypes 3 and 4) has been extracted from pork, boar, and deer meat.
Signs and Symptoms
When they occur, the signs and symptoms of hepatitis E are similar to those of other types of acute viral hepatitis and liver injury. They include:
- Fever
- Fatigue
- Loss of appetite
- Nausea
- Vomiting
- Abdominal pain
- Jaundice
- Dark urine
- Clay-colored stool
- Joint pain
The ratio of symptomatic to asymptomatic infection ranges from 1:2 to 1:13.
Prevention
Prevention of hepatitis E relies primarily on good sanitation and the availability of clean drinking water. Travelers to developing countries can reduce their risk of infection by not drinking unpurified water. Boiling and chlorination of water will inactivate HEV. Avoiding raw pork and venison can reduce the risk of HEV genotype 3 transmission. Immune globulin is not effective in preventing hepatitis E.
No FDA-approved vaccine for hepatitis E is currently available in the United States; however, in 2012 a recombinant vaccine was approved for use in China.
Incidence of Hepatitis E in the United States
Hepatitis E is not commonly acquired in the United States; most cases of symptomatic hepatitis E in the United States occur among people who have traveled to a developing country where hepatitis E is endemic. Sporadic, non-travel-related cases of hepatitis E have been identified in the United States; no clear exposure was identified for these domestically acquired cases. Sporadic cases of hepatitis E in developed countries, including the United States, are primarily caused by HEV genotype 3 and largely affect older men (those >40 years of age).
Post-Exposure
Hepatitis E usually resolves on its own without treatment. There is no specific antiviral therapy for acute hepatitis E. Physicians should offer supportive therapy. Patients are typically advised to rest, get adequate nutrition and fluids, avoid alcohol, and check with their physician before taking any medications that can damage the liver, especially acetaminophen. Hospitalization is sometimes required in severe cases and should be considered for pregnant women.
Few case reports and case series have indicated that modification of immunosuppressive medication and/or use of antiviral drugs may result in spontaneous viral clearance in immunocompromised patients with chronic hepatitis E.
References
Centers for Disease Control and Prevention. https://www.cdc.gov/hepatitis/. Accessed June 19, 2020.
Dan Bunker DNAP, MSNA, CRNA—Dan has worked in the healthcare industry for nearly 30 years. He worked as a registered nurse in the coronary care ICU for 7 years and was a flight nurse with Intermountain’s Life Flight for nearly 10 years. He has been a certified registered nurse anesthetist (CRNA) for 11 years, working in the hospital setting as well as maintaining his own private practice. In addition, he is a professor in the nurse anesthesia program at Westminster College in Salt Lake City, Utah. He has served in various leadership roles within the Utah Association of Nurse Anesthetists (UANA) and is currently the president-elect.




